Abstract
Introduction: Patients with hematologic malignancies (HM) are at high risk for developing concomitant infections given their immunosuppression. Tuberculosis (TB) is a worldwide public health issue which affects developing countries most severely, and within them, patients with decreased immunity are most vulnerable. There are few studies examining the clinical factors associated with development of TB and survival, this is especially true in high-endemic developing countries where previous analysis have considered both microbiologically confirmed and suspected TB.
Objective: Our primary objective was to examining clinical and pathologic factors associated with development of clinically active TB in a cohort of patients with HM and microbiologically confirmed TB. A secondary objective was to analyze factors associated with survival
Methods: This single-center retrospective cohort study included 46 adult patients with HM (Hodgkin Lymphoma, Non-Hodgkin Lymphoma, Multiple Myeloma, Acute Myeloid Leukemia, Acute Lymphoblastic Leukemia, Chronic Lymphocytic Leukemia, Chronic Myeloid Leukemia) and subsequent development of clinically active TB with microbiological confirmation (either through Acid Fast Bacilli stain or culture) at Instituto Nacional de Enfermedades Neoplasicas (INEN) a tertiary cancer center in Peru between January 2006 and September 2015. Patients were divided into two groups based on their HM diagnosis: Lymphomatous (n=32, 69.6%) and Leukemic/myeloma (n=14, 30.4%). Medical records were reviewed, including demographic data, pertinent laboratory data, Charlson Comorbidity Index (CCI), history of previous TB or contact with TB patients, ECOG, viral co-infections, treatment modality and response. Data was analyzed using T-Test and chi-square test, survival curves were estimated by Kaplan-Meier and comparison was done by log-rank test. Multivariate analysis for survival was performed with Cox proportional hazard regression.
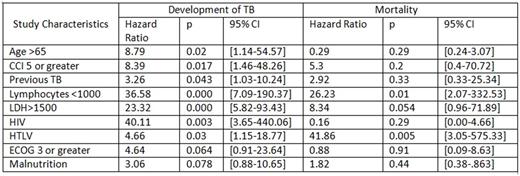
Results: Over the 10-year period we identified 46 adult patients with HM who subsequently developed culture confirmed TB during the observation period. Lymphomatous (L) and Leukemic/Myeloma (LM) subjects had a mean age of 57.03 and 40.93 respectively (p=0.009). LM patients had lower Hemoglobin (8.75 vs 11.18, p=0.003) and higher LDH levels (3134 vs 936, p=0.027). LM diagnosis was also associated with CCI scores less or equal to 4 (OR: 8.76, 95% CI [1.67, 45.88], p=0.005), negative HIV status (OR: 1.33, 95% CI [1.092, 1.629], p=0.004) and lower presence of constitutional symptoms (OR: 0.139, 95% CI [0.033, 0.578], p=0.004). Median times to development of Tuberculosis (dTB) were 4.9 months overall, 3.76 in the LM and 5.26 in the L group, the difference was not statistically significant (p=0.272). Mean overall survival (OS) were 67.94 for LM and 68.73 for L, difference was not statistically significant (p=0.56). In multivariate analysis for the entire cohort, age greater than 65, CCI of 5 or more, Absolute lymphocyte count <1000, LDH>1500, previous TB, presence of HIV and HTLV infection were associated with earlier dTB (see Table). Malnutrition and having an ECOG score of 3 or more were also associated but without statistical significance. HTLV infection and Absolute Lymphocyte Count <1000 were associated with mortality. TB related variables, including: Site of TB, Acid Fast Stain Status and Tuberculosis Treatment Regimen were not associated with mortality.
Conclusions: We have analyzed the first cohort of HM patients with microbiologically confirmed TB in a high prevalence setting and have identified risk factors for development of TB including age, CCI, lymphopenia, high LDH, HIV and HTLV. This study will facilitate the identification of patients with HM at risk of developing TB.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal